What is atherosclerotic cardiovascular disease?

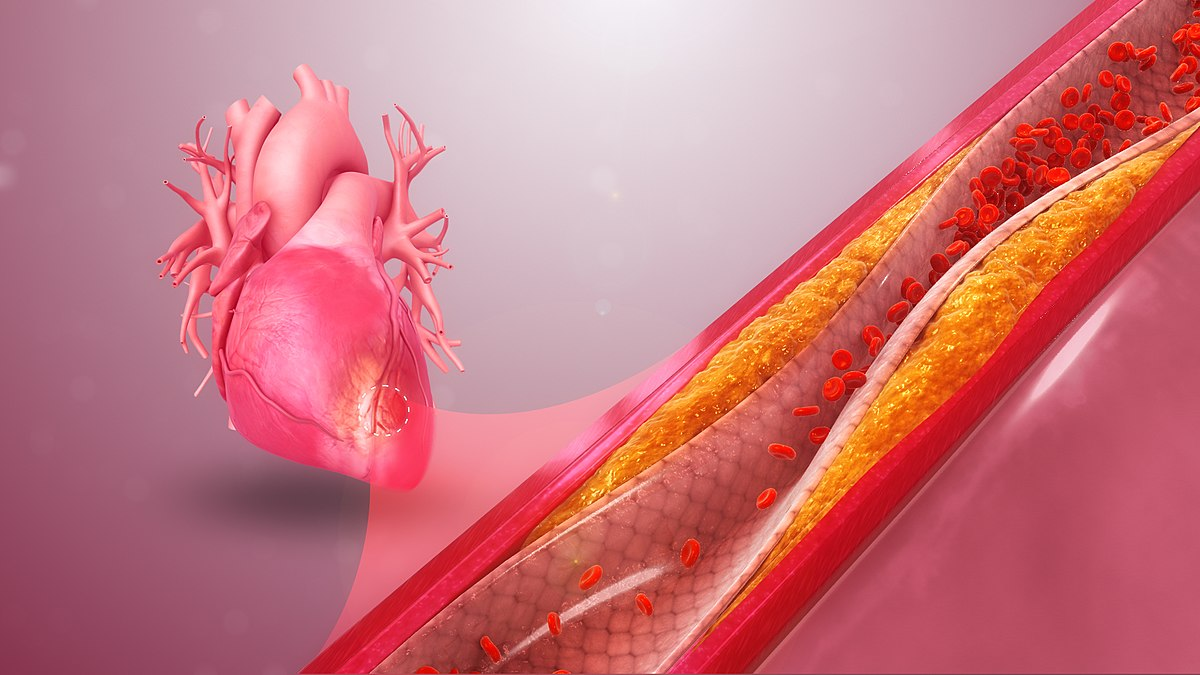
Did you know that heart disease often begins silently in childhood and remains unnoticed for decades? According to the US National Institute of Health, half the population of America in the age group of 45 to 84 has atherosclerosis, yet they are not aware of it. Atherosclerotic cardiovascular disease (ASCVD) is caused by plaque buildup in arterial walls. It is a slowly progressing disease that starts in childhood.
As a result of this deposition of plaque, the arteries become narrow and limit the flow of blood. This further reduces the blood flow to the heart, brain, and other important organs, cutting off their oxygen and nutrient supply. Usually, it causes no noticeable symptoms until it becomes severe.
In this blog post, Gauze includes all you need to know about atherosclerotic cardiovascular disease.
What is atherosclerotic cardiovascular disease?
When plaque builds up in the arterial walls, it causes conditions that include
- Coronary heart disease: myocardial infarction, angina, and coronary artery stenosis
- Cerebrovascular disease: transient ischemic attack, ischemic stroke
- Peripheral artery disease: claudication, carotid artery stenosis
- Aortic atherosclerotic disease: abdominal aortic aneurysm
Risk factors for atherosclerosis are
- High blood pressure
- High cholesterol and triglyceride levels
- Smoking
- Obesity
- Type1 diabetes
- Physical inactivity
- High saturated fat diet
Symptoms of atherosclerosis
Mild atherosclerosis usually does not cause any symptoms. They appear only when the artery is so narrowed or clogged that the blood supply is completely obliterated. Sometimes they may completely block and cause a heart attack or stroke, and the symptoms depend on the arteries affected.
- In the heart arteries, it causes chest pain or pressure.
- In the brain arteries, numbness or weakness in arms or legs, slurred speech, sudden or temporary loss of vision, drooping muscles of the face.
- Pain in arms and legs while walking, low blood pressure in the affected arm or leg.
- In the kidneys, high blood pressure, kidney failure, and aneurysm.
Atherosclerosis and plaque
Let us understand the role of plaque formation in atherosclerosis.
Plaque is a fatty deposit in the arteries, made up of
- Cholesterol
- fatty substance
- cellular waste
- Calcium
- Fibrin (clotting material in blood)
When it deposits in the blood vessel, it thickens the vessel wall and narrows its lumen, causing double damage in our bodies.
A heart attack, stroke, or gangrene occurs if the blood supply to the heart, brain, or extremities is blocked.
How does plaque form?
Injury to the arterial wall due to
- High blood pressure
- Smoking
- High cholesterol
produces white blood cells, which attach to the walls of the artery and lay the foundation of plaque. It tends to form along the medium and large-sized arteries just where they branch.
Stages of atherosclerosis
Atherosclerosis develops in stages over a long period
- Endothelial damage and immune response
The inner lining of a blood vessel (endothelium) is damaged as a result of injury, attracting white blood cells, which move to the site of injury, causing local inflammation.
- Fatty streak formation
A yellow line or patch inside the artery is the first visible sign of atherosclerosis. White blood cells consume cholesterol and break it down, forming patches of foam cells that accumulate at the site of blood vessel damage.
The foam cell’s continued activity erodes the inner lining of the blood vessels (or endothelium).
- Plaque growth
Over time, dead plaque cells and cellular debris build up inside the artery wall, and it doesn’t stay small. To protect the vessel wall, smooth muscle cells move to the site and form a fibrous cap over the plaque. It works like a bandage, making the artery narrow. As the plaque grows, less blood and less oxygen can pass through, starving the heart, brain, and other organs.
- Plaque rupture
Gradually, the fibrous cap ruptures, exposing plaque contents to the bloodstream.
Another possibility is that the cap remains intact. Still, the surrounding endothelial cells become damaged, leading to the formation of a clot that suddenly blocks blood flow and causes a heart attack or stroke.
How is atherosclerosis diagnosed?
After medical history and physical examination come the tests, which include
- Cardiac catheterization: A long, thin tube catheter is passed through the coronary arteries. A dye injected into the artery locates narrowing, blockages, and other abnormalities using an X-ray.
- Doppler Sonography: Detects the flow of blood in the blood vessels by sound waves. Faint or absent sounds indicate a blockage and are used to identify narrowing in blood vessels in the abdomen, neck, or legs.
- Blood pressure comparison: Comparing the blood flow in the ankles and in the arms helps to determine a constriction. Significant differences indicate atherosclerosis.
- MUGA radionuclide angiography: A nuclear scan that detects heart wall movements and the quantity of blood expelled with each heartbeat while a person is at rest.
- Thallium myocardial perfusion scan: A nuclear scan done after exercise and rest, reveals the areas of muscle that are not getting sufficient supply of blood.
- Computerized tomography or CT: What type of X-ray scans for coronary calcification
How is atherosclerosis treated?
Lifestyle changes, medicine, and surgery are the main modalities for its treatment.
1. Lifestyle changes
Changes that reduce the impact of atherosclerosis
- Quitting smoking
- Eating a balanced, low-saturated-fat diet
- Exercising regularly
- Maintaining a healthy weight
- Managing blood pressure and cholesterol.
2. Medicines
Medicines used to treat atherosclerosis belong to groups
- Antiplatelet medicines: Aspirin and clopidogrel are types of medicines that decrease the ability of platelets. In blood to stick together and in form clothes.
- Anticoagulants: Warfarin and heparin are blood thinners that decrease the ability of blood to clot.
- Cholesterol-lowering medicines: Statins like atorvastatin and pravastatin are used to lower lipids in the blood, especially LDL cholesterol.
- Blood pressure medicines: They act in different ways to lower the BP.
3. Surgery
Coronary angioplasty
- A long, thin tube catheter is threaded through a blood vessel into the heart, where a balloon is inflated to enlarge the opening in the vessel to increase the blood flow. Percutaneous coronary intervention (PCI) refers to angioplasty in the coronary arteries. PCI procedures are of several types.
- Balloon angioplasty: A small balloon inflates the blocked artery to open the blockage.
- Atherectomy: A tiny device at the end of the catheter is used to shave off the area inside the artery.
- Laser angioplasty: It uses a laser to remove the blockage.
- Coronary artery stent: A mesh coil is left in the area of blockage and expanded to keep the artery open.
4. Coronary artery bypass
Bypass surgery is done in people with angina due to coronary artery disease. A bypass is created by grafting a piece of healthy vein from another part of the body and attaching it above and below the blocked area of a coronary artery. It allows blood to flow around the blockage. The wings are usually taken from the legs or the chest wall. At times, we may need to bypass more than one artery.
Conclusion
Atherosclerotic cardiovascular disease silently creeps into the cardiovascular system. By the time it shows up, it is late, and damage has already been done. Good news is small, consistent choices such as doing physical activity, eating a balanced diet, staying away from tobacco, and excess alcohol go a long way in maintaining our heart health. Prevention is better than cure, and the only way to stay ahead of the impending threat.
Here to answer all your questions
Yes, while atherosclerosis cannot be completely reversed, many people live long and healthy lives. Having a healthy heart and a healthy lifestyle, regular exercise, a balanced diet, maintaining body weight, quitting smoking, and limiting alcohol, taking appropriate medications prescribed by the doctor, slows the progression of the disease and reduces the risk of complications.
Vitamin C and E.
- Vitamin C is associated with a decrease in the prevalence of coronary artery disease because it supports and improves endothelial function.
- Vitamin E reduces oxidative stress and prevents heart disease.
It is a coronary angiogram or cardiac catheterization. A minimally invasive procedure that gives a view of artery narrowing or blockage. Other tests, like CT coronary angiography, are excellent non-invasive options to detect blockage and plaque buildup. A stress test and ECG can help us assess heart function and rhythm, but they do not pinpoint a specific blockage.
It is best to avoid
- Saturated fats, such as those found in meat, bacon, butter, and full-fat dairy.
- Trans fats are found in hydrogenated oils, fried foods, and processed snacks.
- Tropical oils such as coconut oil, palm oil.
We must choose healthy fats such as olive oil, nuts, seeds, and fatty fish rich in Omega-3.
Vitamin C and E.
- Vitamin C is associated with a decrease in the prevalence of coronary artery disease because it supports and improves endothelial function.
- Vitamin E reduces oxidative stress and prevents heart disease.
Plaque is a fatty, waxy deposit of fat, cholesterol, and other substances in the artery. When calcium, a mineral, deposits in the plaque, it hardens over time. The presence of calcium indicates a more established calcified plaque, which is a sign of atherosclerosis and increased heart attack risk. A coronary calcium scan (CAC score )is often used to measure calcium in coronary arteries to estimate cardiovascular risk.

